November 2018
2018 Annual HEDIS®/QRS Reports
Blue Cross and Blue Shield of Texas (BCBSTX) has a Quality Improvement Program (QIP) to better serve you. The purpose of the QIP is to monitor and improve the care and service our members receive. We focus on encouraging preventive health and safety, and provide education related to chronic conditions.
There is a standard way to measure important areas of care and service called the Health Care Effectiveness Data and Information Set (HEDIS). These measures were developed by the National Committee for Quality Assurance (NCQA). They are widely used to measure health care performance in the U.S.
The Centers for Medicare & Medicaid Services has a similar set of measures, the Quality Rating System (QRS). These measure similar areas of care and are specifically for those members enrolled in marketplace health care plans.
Through the QIP, BCBSTX measures how we are doing against the goals we’ve set. The table below summarizes how we are doing on selected measures.
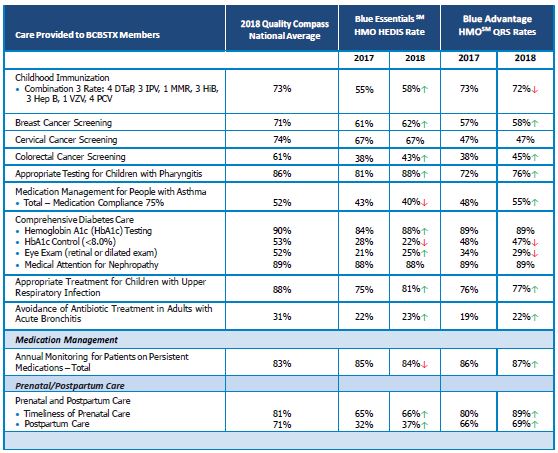
Key improvements in 2018 are seen in both the commercial (Blue Essentials) and retail (Blue Advantage HMO) memberships for:
- Colorectal cancer screening
- Appropriate testing for children with pharyngitis
- Appropriate treatment for children with upper respiratory infections
- Timeliness of prenatal care and postpartum care
The most significant decline from last year fell under Comprehensive Diabetes Care. More specifically, in HbA1c control in our commercial membership and eye exams in our retail membership.
How You Can Help
While BCBSTX provides education and resources to our members, your support in these efforts can positively impact your patient’s compliance with necessary preventive care screenings and routine monitoring of chronic health conditions. An established process to identify gaps in care and dedicated outreach staff are just a couple ways you can improve your patient’s health outcomes.
Results are rounded to the nearest percentage.
HEDIS is a registered trademark of NCQA
