March 2019
Government Programs: New Tool for Verifying Claim Status in Availity®
This notice applies to providers rendering services for the following Blue Cross and Blue Shield of Texas (BCBSTX) government program members:
- Texas Medicaid STAR, STAR Kids and CHIP
- Blue Cross Medicare Advantage (HMO)SM and Blue Cross Medicare Advantage (PPO)SM
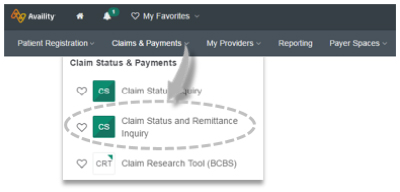
A new claim status tool within the Availity Provider Portal has been added to help with getting claim details online. Instead of using the Claim Status Inquiry tool, government program providers can now obtain claim processing details by using the new Claim Status and Remittance Inquiry tool.
Important claim status information is now available within a few clicks, lessening the need to speak with a Customer Advocate. As a reminder, you must be registered with Availity to use the Claim Status and Remittance Inquiry tool. For registration information, visit availity.com or contact Availity Client Services at 800-282-4548.
How to access and use the new claim status tool via Availity:
- Log in to availity.com
- Select the “Claims & Payment” tab from the main menu and then select “Claim Status and Remittance Inquiry”
- Next select “Claim Status”
- Choose the applicable government program payer from the drop-down list
- Enter the essential provider, patient and claim data
Additional Support
Learn how to use this new Availity tool by attending an Availity 101 training webinar hosted weekly by BCBSTX. If you need assistance or customized training, email our Provider Education Consultant team at PECS@bcbstx.com.
Availity® is a trademark of Availity, LLC, a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSTX. BCBSTX makes no endorsement, representations or warranties regarding any products or services provided by third-party vendors such as Availity. If you have any questions about the products or services provided by such vendors, you should contact the vendor(s) directly.
