Page 16 - 2021 Summer Enrollment
P. 16
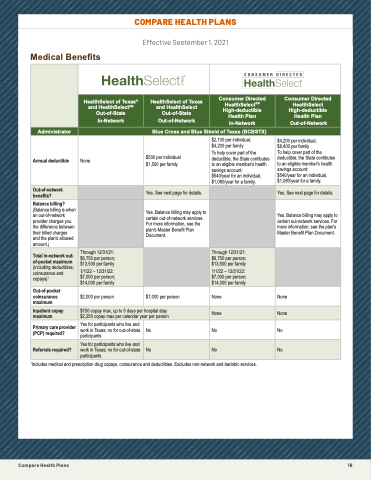
EFFECTIVE SEPTEMBER 1, 2021
This chart shows your share of costs for commonly used medical, mental health, prescription drug and diabetes supply benefits in
® SM
the HealthSelect of Texas and Consumer DiCreOcteMd PHeAalRthSEeleHctEAplLanTs.HFoPr iLn-dAepNthSinformation about eligibility, services that are
covered and not covered, and how benefits are paid, view the Master Benefits Plan Document (MBPD) on your plan’s website. If there is a conflict between the MBPD, MBPD Amendments and this chart, the MBPD and its Amendments will control.
Effective September 1, 2021
Blue Cross and Blue Shield of Texas (BCBSTX) administers medical and mental health benefits in both plans. OptumRx, an affiliate of UnitedHealthcare, manages prescription drug benefits for the plans. As administrators, they process claims and oversee the provider MnetweodrkiscanadldrBugefonrmeulfiarites. ERS designs the benefits and pays the claims.
Service
Allergy treatment Ambulance services
HealthSelect of Texas® and HealthSelectSM Out-of-State
In-Network
HealthSelect of Texas and HealthSelect Out-of-State
Out-of-Network
Consumer Directed HealthSelectSM High-deductible Health Plan
In-Network
Consumer Directed HealthSelect High-deductible Health Plan
Out-of-Network
® CoHveraeldthaSt 1e0l0e%ctifoafdmTeinxisatesred
in a pahnydsicHiaena’slothffiSce;l2e0c%tSM
coinsuranOcue tin-oafn-ySottahter
outpatient location
In-Network
HealthSelect of Texas 40% caonindsuHraenaceltahfSteer alencnutal d e d u c t i b l Oe i u s t m - o e f t - S t a t e
Out-of-Network
20% coinsurance; annual
Consumer Directed
HealthSelectSM
20% coinsurance after annual
High-deductible
deductible is met
Health Plan
In-Network
20% coinsurance after annual
Consumer Directed
HealthSelect
40% coinsurance after annual
High-deductible
deductible is met
Health Plan
Out-of-Network
20% coinsurance after annual
Administrator
(for emergencies)
20% coinsurance
Blue Cross and Blue Shield of Texas (BCBSTX)
deductible does not apply deductible is met in-network deductible is met
Bariatric surgery2 Annual deductible
Chiropractic care
• Deductible: $5,000
• Coinsurance: 20%
• Lifetime max: $13,000
None
• Without office visit: 20%
coinsurance
• With office visit: $40 copay plus 20% coninsurance
Not covered
$500 per individual
$1,500 per family
40% coinsurance after annual deductible is met.
Maximum benefits of $75 per
$2,100 per individual,
To help cover part of the deductible, the State contibutes to an eligible member's health 2s0a%vincgosinascucroaunncte: after annual d$e5d4u0c/ytiebaler ifsormaent.individual,
$1,080/year for a family. Maximum benefits of $75 per
$4,200 per family Not covered
$4,200 per individual,
$8,400 per family Not covered
To help cover part of the
deductible, the State contibutes
to an eligible member's health
savings account:
40% coinsurance after annual
d$e5d4u0c/ytiebaler ifsormaent.individual,
$1,080/year for a family. Maximum benefits of $75 per
Out-of-network benefits?
• Maximum benefits of $75 per visit and maximum of 30 visits
visit and maximum of 30 visits
Yes. See next page for details. per calendar year
visit and maximum of 30 visits per calendar year
visit and maximum of 30 visits
Yes. See next page for details. per calendar year
Balance billing?
(Balance billing is when
Diabetes
an out-of-network
equipment2 provider charges you
the difference between Dthieairbbeitllesd scuhaprpgleiess and the plan's allowed Damiaogunnot.s)tic X-rays
per calendar year
20% coinsurance;
see page 20 for details.
20% coinsurance
40% coinsurance after annual Yes. Balance billing may apply to deductible is met;
certain out-of-network services. see page 20 for details.
For more information, see the
plan's Master Benefit Plan
See page 2 40% coinsurance after annual
Document.
20% coinsurance after annual deductible is met;
see page 20 for details.
0 for details.
20% coinsurance after annual
40% coinsurance after annual dYedsu. cBtaiblalenicsembeillti;ng may apply to sceertapiangoeu2t-0nefotwr doerktasilesr.vices. For more information, see the plan's Master Benefit Plan Document.
40% coinsurance after annual
and lab tests
Total in-network out- Diagnostic
of-pocket maximum mammography
(including deductibles,
Durable medical
coinsurance and
equipm1ent2 copays)
Facility-based
Through 12/31/21:
$6,750 per person; Covered at 100% $13,500 per family
1/1/22 – 12/31/22: 20% coinsurance $7,000 per person;
$14,000 per family
deductible is met
40% coinsurance after annual deductible is met
40% coinsurance after annual deductible is met
deductible is met Through 12/31/21:
2$06%,75c0oipnesrupraenrscoena;fter annual d$e1d3u,5c0ti0blpeeisr fmametily
210/1%/2c2o–in1s2u/r3a1n/c2e2:after annual d$e7d,0u0c0tibplerispemrseot n;
$14,000 per family
deductible is met
40% coinsurance after annual deductible is met
40% coinsurance after annual deductible is met
Emergencies: 20% coinsurance;
annual deductible does not $7,000 per person
apply.
Non emergencies: 40%
care (non FSER)
1Idneclpuadretms emnetsdical and prescription drug copays, coinsurance anpdlusde4d0u%ctciboliens.uEraxnccluedaeftsernaonn-nueatlwork and bariatric services.
Emergencies: 20% coinsurance
after annual in-network None
deductible is met.
Non emergencies: 40%
No
Emergencies: 20% coinsurance
after annual in network
network deductible is met.
Emergencies: 20% coinsurance after annual in-network deductible is met.
Non-emergencies: 40% coinsurance after annual out-of- network deductible is met.
40% coinsurance after annual deductible is met
pOruotv-oidf-eproscket (croaidniosluorgaisntcse, pmaathxoimlougmists and labs,
physicians etc.)
$2,000 per person 20% coinsurance
Yes for participants who live and
work in Texas; no for out-of-state
$150 copay plus 20% coinsurance
20% coinsurance
None
20% coinsurance after annual
deductible is met No
anesthesiologists,
Inpatient copay
emergency room
maximum
$750 copay max, up to 5 days per hospital stay
coinsurance after annual
$2,250 copay max per calendar year per person deductible is met
-
None
-
coinsurance after annual out-of- None
network deductible is met.
Primary care provider
Emergencies: $150 copay plus No
(PCP) required? Facility emergency
participants
$150 copay plus 20%
20% coinsurance (If admitted, copay will apply to hospital
-
and hospital-affiliated
Referrals required?
freestanding emergency
Yes for participants who live and coinsurance
work in Texas; no for out-of-state (If admitted, copay will apply to participants
hospital copay.)
copay.) Annual deductible does
No
not apply.
Non-emergencies: $150 copay
20% coinsurance after annual
No
deductible is met
deductible is met.
No
Non-emergencies: 40%
-
coinsurance after annual out-of-
Freestanding emergency room facility
Habilitation and rehabilitation services - outpatient therapy (including
out-of-network deductible is met.
Emergencies: $300 copay plus 20% coinsurance; annual deductible does not apply.
Non-emergencies: $300 copay plus 40% coinsurance after annual out-of-network deductible is met.
40% coinsurance after annual deductible is met
20% coinsurance after annual deductible is met
20% coinsurance after annual deductible is met
2
physical therapy, occupational therapy and speech therapy)
Compare Health Plans
16
.
Preauthorization may be required